Overview of Immune System
1. Introduction to Immune System
The immune system is a complex network of cells, tissues, and organs that work together to protect the body from harmful pathogens such as bacteria, viruses, fungi, and parasites. In addition to defending against infections, the immune system also plays a critical role in eliminating damaged or abnormal cells, such as cancerous cells. The immune system has two main types of defenses: innate immunity and adaptive immunity, each with its own specialized functions and characteristics.
Figure 1. Innate Immunity Versus Adaptive Immunity (Source: Biorender.com)
Innate Immunity: The body's first line of defense, offering immediate but nonspecific protection against pathogens.
Adaptive Immunity: A more specific and adaptable defense mechanism that is activated upon exposure to pathogens and improves with subsequent exposures.
Figure 2. Stages of Adaptive Immune Response (Source: Biorender.com)
2. Components of the Immune System
The immune system includes several key components, each playing a vital role in defending the body:
a) Primary Organs:
Bone Marrow: The site of origin for all immune cells. It produces white blood cells, red blood cells, and platelets.
Thymus: A small organ located in the chest, where T lymphocytes (T cells) mature before being released into the bloodstream.
b) Secondary Organs:
Lymph Nodes: Distributed throughout the body, lymph nodes filter lymph fluid and trap pathogens. They are also sites where immune cells interact with antigens.
Spleen: Filters blood, removes old red blood cells, and activates immune responses to blood-borne pathogens.
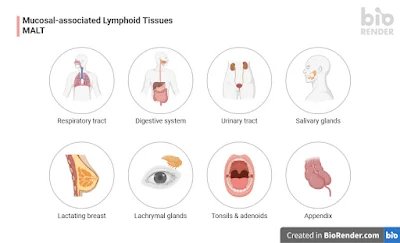
Mucosal-associated lymphoid tissues (MALT): These include structures like the tonsils, Peyer’s patches in the intestines, and other lymphoid tissues found in mucosal surfaces, playing an important role in immune responses to pathogens entering through mucosal surfaces.
Figure 7. Mucosal-associated lymphoid tissues (MALT) (Source: Biorender.com)
c) Cells of the Immune System:
Leukocytes (White Blood Cells): Key players in immune defense, including various subtypes:
Neutrophils: The first responders to infection and the most abundant white blood cells.
Macrophages: Engulf and digest pathogens and dead cells; also play a role in activating adaptive immunity.
Dendritic Cells: Serve as antigen-presenting cells (APCs), displaying antigens to T cells and initiating adaptive immunity.
Natural Killer (NK) Cells: Specialized to kill virus-infected cells and tumor cells.
Lymphocytes: Include B cells and T cells, which play a central role in adaptive immunity.
d) Molecules of the Immune System:
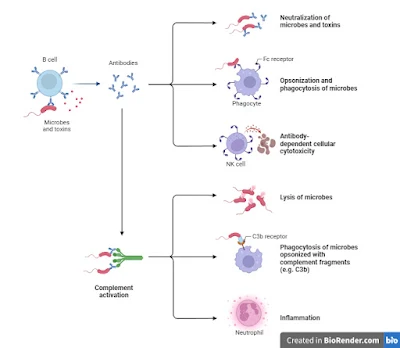
Antibodies (Immunoglobulins): Produced by B cells, antibodies bind to pathogens and neutralize them or mark them for destruction.
Cytokines: Small signaling molecules that regulate immune cell function, inflammation, and hematopoiesis.
Complement Proteins: A group of proteins that enhance the ability of antibodies and phagocytic cells to clear pathogens.
3. Types of Immunity
a) Innate Immunity
Innate immunity is the body’s first line of defense, activated immediately after pathogen detection. It is nonspecific and includes the following:
Physical Barriers.: These are the first defense against pathogens and include the skin, mucous membranes, and secretions like tears and saliva.
Phagocytic Cells: These cells engulf and digest pathogens. Key phagocytes include neutrophils, macrophages, and dendritic cells.
Inflammation: A localized response to infection characterized by redness, swelling, heat, and pain, aimed at recruiting immune cells to the site of infection.
Natural Killer (NK) Cells: Specialized cells that detect and kill infected or abnormal cells, particularly virus-infected cells.
Complement System: A group of proteins that can kill pathogens directly or mark them for destruction by phagocytes.
Key Features of Innate Immunity:
- Rapid Response: Innate immunity is activated within minutes to hours after infection.
- Nonspecific: It does not target specific pathogens but rather responds to general features shared by many pathogens (e.g., bacterial cell walls).
- No Memory: Once an infection is cleared, innate immunity does not retain any specific information about the pathogen for future encounters.
b) Adaptive Immunity
Adaptive immunity is more specific and takes longer to develop but is highly effective and provides long-lasting protection. Key features of adaptive immunity include:
- Specificity: Adaptive immunity targets specific pathogens with high precision.
- Memory: Adaptive immunity remembers pathogens it has encountered, enabling a faster and more efficient response if the pathogen is encountered again.
The adaptive immune response involves B cells and T cells, which respond to specific pathogens and provide lasting immunity.
B Cells: B cells are responsible for the production of antibodies. When activated by an antigen, B cells differentiate into plasma cells that secrete antibodies. These antibodies bind to pathogens, neutralizing them or marking them for destruction by other immune cells.
T Cells: T cells are involved in recognizing and responding to infected or abnormal cells:
Figure 9.TH1 Cells Help Macrophages Kill Intracellular Bacteria (Source: Biorender.com)
- Helper T Cells (CD4+): Assist B cells in producing antibodies and activate cytotoxic T cells and macrophages.
- Cytotoxic T Cells (CD8+): Directly kill infected or cancerous cells by recognizing specific antigens presented on the cell surface.
- Regulatory T Cells: Regulate immune responses to prevent excessive reactions or autoimmunity.
Key Features of Adaptive Immunity:
4. Antigen Presentation and Immune Activation
Antigen Presentation: The immune system identifies pathogens through molecules called antigens. Antigens are often foreign proteins or polysaccharides present on the surface of pathogens.
MHC Molecules: Antigens are presented on the surface of cells by proteins called major histocompatibility complex (MHC) molecules. There are two types of MHC molecules:
- MHC Class I: Present on all nucleated cells and recognized by cytotoxic T cells (CD8+).
- MHC Class II: Present on antigen-presenting cells (APCs) like dendritic cells and macrophages and recognized by helper T cells (CD4+).
When an APC presents an antigen via MHC molecules, T cells recognize and bind to it, triggering an immune response.
5. Immune Memory
One of the most important aspects of adaptive immunity is the formation of immune memory. After the immune system successfully combats a pathogen, memory B cells and memory T cells remain in the body for years, or even a lifetime. If the same pathogen enters the body again, these memory cells quickly recognize it and mount a faster, stronger response.
This principle is the basis of vaccination, where an organism is exposed to a harmless form of a pathogen to trigger the production of memory cells without causing illness.
6. Disorders of the Immune System
Immune system dysfunction can lead to a variety of disorders:
- Autoimmune Diseases: Conditions where the immune system mistakenly attacks the body’s own tissues [e.g., rheumatoid arthritis, Systemic lupus erythematosus (SLE), type-1 diabetes, psoriasis, coeliac disease, multiple sclerosis].
- Immunodeficiencies: Disorders that impair the immune system, making individuals more susceptible to infections. HIV/AIDS is a well-known immunodeficiency. It can be futher divided into primary immunodeficiencies and severe combined immunodeficiencies. The majority of primary immunodeficiency cases are identified in young children, and patients are often more susceptible to infections. However, severe combined immunodeficiencies (SCIDs) are a category of uncommon, monogenic disorders characterised by an early start and a substantial inhibition in T cell development.
- Hypersensitivity: Allergic reactions occur when the immune system overreacts to harmless substances such as pollen, food,or drugs. Common allergens includes medication, venoms from insect sting and bites, contact allergies from metal or fragrance, mold, house dust mites, pets and animals from farms, etc.
7. Vaccination and Immunization
Vaccination is a medical intervention that stimulates the immune system to develop protection against pathogens. Vaccines contain weakened or inactivated pathogens or pathogen components that do not cause disease but stimulate an immune response.
Types of vaccines:
- Live Attenuated (weakened or inactivated) Vaccines: Contain weakened pathogens that can still replicate but cannot cause disease (e.g., measles, mumps, rubella, influeza, oral polio, typhoid, Japanese encephalities, Bacillus Calmette-Guerin (BCG), varicella zoster, yellow fever, and so on).
- Killed whole organism: Contain killed pathogens (e.g., polio vaccine, influenza, Japanese encephalitis, hepatitis A, rabies, Whole-cell pertusis).
- Subunit Vaccines (purified protein, recombinant protein, polysachharide, peptide) : Contain pieces of pathogens, such as proteins or sugars (e.g., hepatitis B vaccine, Pertussis, influenza, meningococcal, penumococcal, typhoid).
- Toxoid: Toxoids (e.g., diphtheria and tetanus vaccines) are non-toxic bacterial toxins that still have the ability to stimulate antitoxin production.
- Virus like particles (VLPs): Virus-like particles (VLPs) are particles that self-assemble as a result of the expression of proteins encoding capsids, cores, or envelopes of viruses, or even preparations of monolayered particles obtained from a multilayered virus. e.g. Human papillomavirus vaccines
- Outer membrane vesicle: Spherical buds derived from outer membrane of Gram-negative bacteria filled with periplasmic content. e.g. Group B meningococcal vacccine
- Protein-polysachharide conjugate:Polysaccharide vaccines for Haemophilus influenzae type b (Hib) were first used in 1985, but they were quickly replaced by protein-polysaccharide conjugate vaccines in 1989. These vaccines contained the Hib polysaccharide polyribosyl ribitol phosphate chemically conjugated to a protein carrier, such as diphtheria toxoid, tetanus toxoid, or meningococcal outer membrane protein.
- Viral vectored vaccines:Viral vector vaccines remain one of the finest techniques for induction of substantial humoral and cellular immunity against human illnesses.Numerous viruses from various families and origins, such as vesicular stomatitis virus, rabies virus, parainfluenza virus, measles virus, Newcastle disease virus, influenza virus, adenovirus, and poxvirus, are regarded as prominent viral vectors. ERVEBO® is a replication-competent, live, attenuated recombinant vesicular stomatitis virus (VSV) used to prevent Ebola virus infection.
- Nuclei Acid Vaccine: Nucleic acid vaccines are a type of genetic vaccine that utilize genetic material, specifically DNA or RNA, to instruct cells in the body to produce a protein associated with a pathogen, which then triggers an immune response. These vaccines are distinct from traditional vaccines, which usually contain inactivated or attenuated pathogens, or proteins derived from pathogens.
The two main types of nucleic acid vaccines are:
DNA Vaccines: Contain a small, circular piece of DNA that encodes the target antigen.
RNA Vaccines: Contain mRNA (messenger RNA) that encodes the target antigen. For instance, the genetic material, RNA in the case of Moderna and Pfizer/BioNTech vaccines, encodes a particular viral protein. The protein is further identified by the immune system triggering a specific response as on the case of SARS-CoV-2 infection. - Bacterial vectored vaccines: These are a type of genetically modified vaccine where harmless bacteria are used as vectors (carriers) to deliver antigens from a pathogen into the body, stimulating an immune response. These vaccines utilize bacteria that have been engineered to carry and express a gene (often from a virus or other pathogen) that encodes an antigen. When the vector bacteria are introduced into the body, they deliver the antigen to the immune system, triggering a response that prepares the body for future encounters with the pathogen. However, these are in due course of their experimental phases.
- Antigen-presenting cells (APCS).:Using APCs as a vaccine strategy, known as APC-based vaccines, is an innovative and promising approach in immunotherapy and vaccine development. This method exploits the natural function of APCs, enhancing their ability to present antigens in a more efficient and targeted way, potentially leading to stronger and more durable immune responses against various pathogens, including viruses, bacteria, and even tumors. However, these are also in their experimental phase.
Vaccines provide active immunity, as the body’s immune system responds to the pathogen or pathogen component in the vaccine, while passive immunity involves the transfer of antibodies (e.g., through breast milk or intravenous immunoglobulin). In addition to the well-established vaccine platforms, such as inactivated, live attenuated, subunit, and nucleic acid vaccines, a variety of experimental vaccine types are being actively researched and developed. These innovative approaches aim to address unmet medical needs, improve immune responses, and overcome limitations of current vaccine strategies. These experimental vaccine types represent the cutting edge of immunology and vaccine development. They offer new avenues for enhancing vaccine efficacy, targeting previously hard-to-reach diseases, and creating more efficient immunization strategies. While many of these vaccines are still in the experimental or clinical trial phases, they hold the promise of expanding our arsenal of vaccines to combat emerging infectious diseases, cancers, and other complex health challenges. Further research and clinical trials will help refine these vaccine technologies and assess their safety, efficacy, and broad applicability.
References
- Abbas, A.K., Lichtman, A.H., & Pillai, S. (2015). Cellular and Molecular Immunology (9th ed.). Elsevier.
- https://app.biorender.com/biorender-templates/figures/all
- Janeway, C.A., et al. (2001). Immunobiology: The Immune System in Health and Disease. Garland Science.
- Murphy, K., Travers, P., & Walport, M. (2008). Janeway's Immunobiology. Garland Science.
- Medzhitov, R. (2001). Toll-like receptors and innate immunity. Nature Reviews Immunology, 1(2), 135-145.
- https://www.nature.com/subjects/autoimmune-diseases
- https://www.nature.com/subjects/primary-immunodeficiency-disorders
- Fischer, A., Notarangelo, L., Neven, B. et al. Severe combined immunodeficiencies and related disorders. Nat Rev Dis Primers 1, 15061 (2015). https://doi.org/10.1038/nrdp.2015.61
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Overview: Allergies. [Updated 2023 Aug 8]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK447112/
- Pumpens P, Pushko P. Virus-like particles, a comprehensive guide. Boca Raton, FL: CRC Press; 2022.
- https://www.nature.com/articles/s41577-020-00479-7/figures/2
- Schwechheimer, C., Kuehn, M. Outer-membrane vesicles from Gram-negative bacteria: biogenesis and functions. Nat Rev Microbiol 13, 605–619 (2015). https://doi.org/10.1038/nrmicro3525
- https://www.cdc.gov/ebola/hcp/vaccines/index.html
- https://www.immunology.org/public-information/vaccine-resources/covid-19/covid-19-vaccine-infographics/types-covid19-vaccines







No comments:
Post a Comment